Doctors in Sc Who Accept Family Planning Medicaid
1. Medicaid is the nation's public health insurance program for people with low income
Medicaid is the nation's public health insurance program for people with low income. The Medicaid program covers 1 in five Americans, including many with complex and costly needs for care. The program is the principal source of long-term intendance coverage for Americans. The vast bulk of Medicaid enrollees lack access to other affordable health insurance. Medicaid covers a wide array of wellness services and limits enrollee out-of-pocket costs. Medicaid finances nearly a fifth of all personal health intendance spending in the U.S., providing significant financing for hospitals, community health centers, physicians, nursing homes, and jobs in the wellness care sector. Title Nineteen of the Social Security Act and a big body of federal regulations govern the program, defining federal Medicaid requirements and land options and authorities. The Centers for Medicare and Medicaid Services (CMS) within the Department of Wellness and Human Services (HHS) is responsible for implementing Medicaid (Figure 1).
Effigy 1: Medicaid plays a primal part in our health care system.
ii. Medicaid is structured as a federal-state partnership
Subject to federal standards, states administer Medicaid programs and accept flexibility to determine covered populations, covered services, health care delivery models, and methods for paying physicians and hospitals. States can also obtain Section 1115 waivers to test and implement approaches that differ from what is required by federal statute merely that the Secretary of HHS determines advance program objectives. Because of this flexibility, in that location is pregnant variation across state Medicaid programs.
The Medicaid entitlement is based on two guarantees: first, all Americans who encounter Medicaid eligibility requirements are guaranteed coverage, and second, states are guaranteed federal matching dollars without a cap for qualified services provided to eligible enrollees. The match rate for well-nigh Medicaid enrollees is determined by a formula in the police force that provides a match of at least l% and provides a higher federal lucifer charge per unit for poorer states (Figure 2).

Figure 2: The bones foundations of Medicaid are related to the entitlement and the federal-land partnership.
3. Medicaid coverage has evolved over time
Under the original 1965 Medicaid law, Medicaid eligibility was tied to cash assistance (either Assistance to Families with Dependent Children (AFDC) or federal Supplemental Security Income (SSI) starting in 1972) for parents, children and the poor aged, blind and people with disabilites. States could opt to provide coverage at income levels higher up cash assistance. Over fourth dimension, Congress expanded federal minimum requirements and provided new coverage options for states especially for children, significant women, and people with disabilities. Congress besides required Medicaid to help pay for premiums and cost-sharing for low-income Medicare beneficiaries and allowed states to offer an option to "purchase-in" to Medicaid for working individuals with disabilities. Other coverage milestones included severing the link betwixt Medicaid eligibility and welfare in 1996 and enacting the Children's Health Insurance Plan (Scrap) in 1997 to cover depression-income children to a higher place the cutting-off for Medicaid with an enhanced federal lucifer rate. Post-obit these policy changes, for the first time states conducted outreach campaigns and simplified enrollment procedures to enroll eligible children in both Medicaid and Scrap. Expansions in Medicaid coverage of children marked the beginning of later reforms that recast Medicaid equally an income-based health coverage program.
In 2010, as part of a broader health coverage initiative, the Affordable Care Deed (ACA) expanded Medicaid to nonelderly adults with income upward to 138% FPL ($17,236 for an individual in 2019) with enhanced federal matching funds (Figure 3). Prior to the ACA, individuals had to be categorically eligible and run into income standards to qualify for Medicaid leaving most low-income adults without coverage options as income eligibility for parents was well below the federal poverty level in near states and federal constabulary excluded adults without dependent children from the program no matter how poor. The ACA changes effectively eliminated categorical eligibility and allowed adults without dependent children to exist covered; however, equally a effect of a 2012 Supreme Court ruling, the ACA Medicaid expansion is effectively optional for states. Under the ACA, all states were required to modernize and streamline Medicaid eligibility and enrollment processes. Expansions of Medicaid have resulted in historic reductions in the share of children without coverage and, in the states adopting the ACA Medicaid expansion, sharp declines in the share of adults without coverage. Many Medicaid adults are working, but few have access to employer coverage and prior to the ACA had no options for affordable coverage.

Effigy three: Medicaid has evolved over fourth dimension to meet changing needs.
four. Medicaid covers one in v Americans and serves various populations
Medicaid provides health and long-term intendance for millions of America's poorest and most vulnerable people, acting as a high risk pool for the private insurance marketplace. In FY 2017, Medicaid covered over 75 meg depression-income Americans. As of Feb 2019, 37 states accept adopted the Medicaid expansion. Data as of FY 2017 (when fewer states had adopted the expansion) show that 12.6 meg were newly eligible in the expansion grouping. Children account for more than four in x (43%) of all Medicaid enrollees, and the elderly and people with disabilities account for about ane in four enrollees.
Medicaid plays an peculiarly critical role for certain populations covering: nearly half of all births in the typical state; 83% of poor children; 48% of children with special health care needs and 45% of nonelderly adults with disabilities (such equally physical disabilities, developmental disabilities such as autism, traumatic brain injury, serious mental disease, and Alzheimer's disease); and more than than half-dozen in ten nursing home residents. States tin opt to provide Medicaid for children with meaning disabilities in college-income families to fill up gaps in individual health insurance and limit out-of-pocket financial burden. Medicaid also assists most 1 in v Medicare beneficiaries with their Medicare premiums and cost-sharing and provides many of them with benefits non covered by Medicare, peculiarly long-term care (Figure 4).
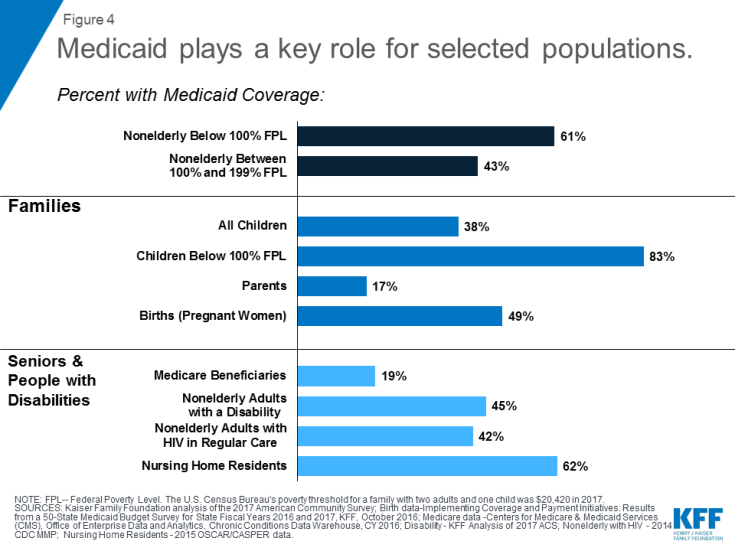
Figure 4: Medicaid plays a key role for selected populations.
five. Medicaid covers a broad range of health and long-term care services
Medicaid covers a broad range of services to accost the diverse needs of the populations information technology serves (Figure 5). In addition to roofing the services required by federal Medicaid law, many states elect to cover optional services such every bit prescription drugs, concrete therapy, eyeglasses, and dental intendance. Coverage for Medicaid expansion adults contains the ACA's 10 "essential wellness benefits" which include preventive services and expanded mental health and substance employ treatment services. Medicaid plays an important office in addressing the opioid epidemic and more broadly in connecting Medicaid beneficiaries to behavioral wellness services. Medicaid provides comprehensive benefits for children, known as Early Periodic Screening Diagnosis and Treatment (EPSDT) services. EPSDT is especially of import for children with disabilities because individual insurance is often inadequate to meet their needs. Unlike commercial health insurance and Medicare, Medicaid also covers long-term intendance including both nursing home care and many dwelling and community-based long-term services and supports. More than one-half of all Medicaid spending for long-term care is now for services provided in the dwelling or customs that enable seniors and people with disabilities to live independently rather than in institutions.
Given that Medicaid and CHIP enrollees have limited ability to pay out-of-pocket costs due to their pocket-size incomes, federal rules prohibit states from charging premiums in Medicaid for beneficiaries with income less than 150% FPL, prohibit or limit cost sharing for some populations and services, and limit total out-of-pocket costs to no more than than 5% of family unit income. Some states have obtained waivers to accuse higher premiums and toll sharing than allowed under federal rules. Many of these waivers target expansion adults simply some also apply to other groups eligible through traditional eligibility pathways.

Figure v: Medicaid'south benefits reflect the needs of the population it serves.
half-dozen. Well-nigh Medicaid enrollees go care through private managed intendance plans
Over two-thirds of Medicaid beneficiaries are enrolled in private managed care plans that contract with states to provide comprehensive services, and others receive their care in the fee-for-service system (Effigy six). Managed intendance plans are responsible for ensuring access to Medicaid services through their networks of providers and are at financial take chances for their costs. In the past, states limited managed care to children and families, merely they are increasingly expanding managed care to individuals with complex needs. Close to one-half united states at present embrace long-term services and supports through take chances-based managed care arrangements. Most states are engaged in a variety of delivery system and payment reforms to command costs and improve quality including implementation of patient-centered medical homes, meliorate integration of concrete and behavioral health care, and development of "value-based purchasing" approaches that tie Medicaid provider payments to health outcomes and other performance metrics. Customs health centers are a key source of primary care, and safety-net hospitals, including public hospitals and academic medical centers, provide a lot of emergency and inpatient hospital care for Medicaid enrollees.
Medicaid covers a continuum of long-term services and supports ranging from home and community-based services (HCBS) that allow persons to live independently in their own homes or in other community settings to institutional care provided in nursing facilities (NFs) and intermediate care facilities for individuals with intellectual disabilities (ICF-IDs). In FY 2016, HCBS represented 57 percent of total Medicaid expenditures on LTSS while institutional LTSS represented 43 percentage. This is a dramatic shift from 1995 (two decades earlier) when institutional settings accounted for 82 percent of national Medicaid LTSS expenditures.

Figure 6: Over two-thirds of all Medicaid beneficiaries receive their intendance in comprehensive take a chance-based MCOs.
7. Medicaid facilitates admission to care
A big body of research shows that Medicaid beneficiaries have far better access to care than the uninsured and are less likely to postpone or get without needed care due to cost. Moreover, rates of access to care and satisfaction with care among Medicaid enrollees are comparable to rates for people with individual insurance (Effigy 7). Medicaid coverage of depression-income significant women and children has contributed to dramatic declines in infant and child mortality in the U.S. A growing torso of enquiry indicates that Medicaid eligibility during childhood is associated with reduced teen mortality, improved long-run educational attainment, reduced disability, and lower rates of hospitalization and emergency department visits in later life. Benefits also include 2d-order fiscal furnishings such as increased revenue enhancement collections due to college earnings in adulthood. Research findings show that state Medicaid expansions to adults are associated with increased access to care, improved self-reported health, and reduced bloodshed among adults.
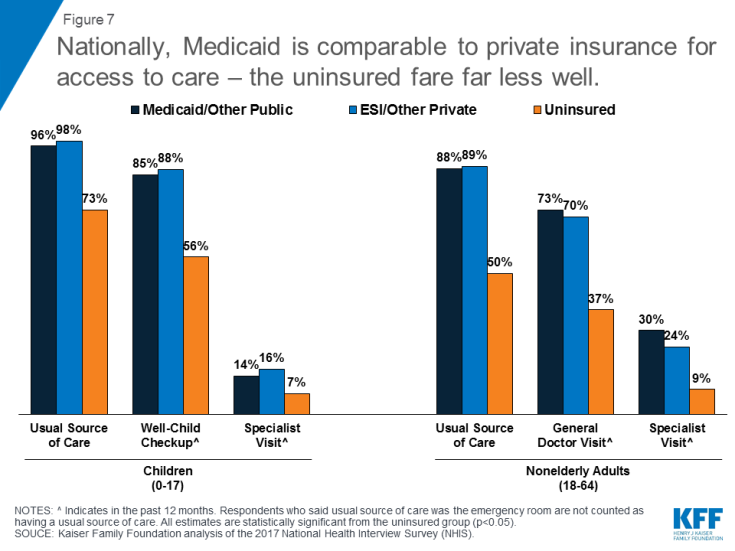
Figure 7: Nationally, Medicaid is comparable to individual insurance for admission to intendance – the uninsured fare far less well.
Gaps in access to sure providers, especially psychiatrists, some specialists, and dentists, are ongoing challenges in Medicaid and often in the health organization more broadly due to overall provider shortages, and geographic maldistribution of health care providers. Notwithstanding, depression Medicaid payment rates take long been associated with lower md participation in Medicaid, especially among specialists. Managed care plans, which at present serve virtually Medicaid beneficiaries, are responsible under their contracts with states for ensuring adequate provider networks. In that location is no evidence that physician participation in Medicaid is declining. In a 2015 survey, 4 in 10 principal care providers who accepted Medicaid reported seeing an increased number of Medicaid patients since January 2014, when the coverage expansions in the ACA took full result.
Medicaid covers people who are struggling with opioid habit and enhances country chapters to provide access to early interventions and handling services. The Medicaid expansion, with enhanced federal funding, has provided states with additional resources to encompass many adults with addictions who were previously excluded from the plan. Medicaid covers 4 in 10 nonelderly adults with opioid habit.
viii. Medicaid is jointly financed by states and the federal government
Medicaid is financed jointly past the federal regime and states. The federal government matches state Medicaid spending. The federal match charge per unit varies past state based on a federal formula and ranges from a minimum of 50% to nearly 75% in the poorest state. Nether the ACA, the federal match rate for adults newly eligible was 100% for 2014-2016, phasing downward gradually to 90% in 2020 and thereafter (93% in 2019). The federal matching construction provides states with resources for coverage of their depression-income residents and too permits land Medicaid programs to respond to demographic and economical shifts, changing coverage needs, technological innovations, public health emergencies such equally the opioid addiction crunch, and disasters and other events across states' control. The guaranteed availability of federal Medicaid matching funds eases monetary pressures on states during recessionary periods when enrollment rises. Federal matching rates do not automatically adjust to economical shifts but Congress has twice raised them temporarily during downturns to strengthen back up for states.
Total federal and land Medicaid spending was $577 billion in FY 2017. Medicaid is the third-largest domestic program in the federal budget, later on Social Security and Medicare, accounting for nine.5% of federal spending in FY 2017. In 2017, Medicaid was the 2d-largest item in country budgets, after elementary and secondary education (Effigy 8).
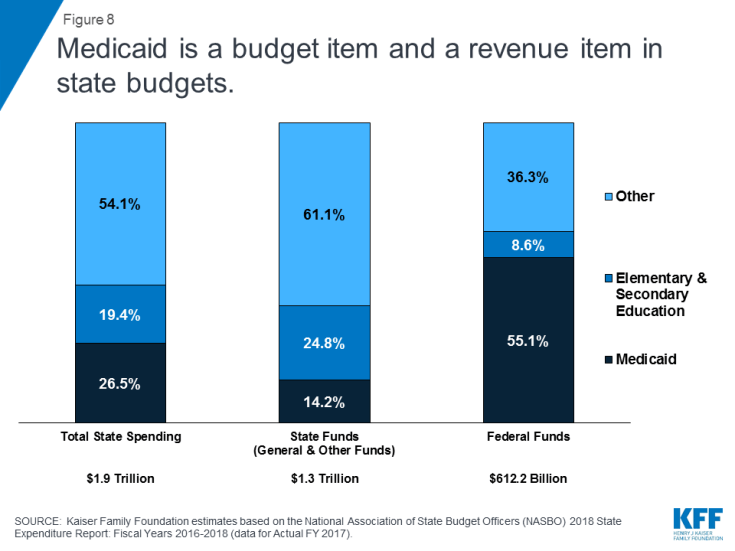
Effigy viii: Medicaid is a budget item and a revenue detail in land budgets.
Federal Medicaid matching funds are the largest source of federal revenue (55.ane%) in state budgets. Bookkeeping for land and federal funds, Medicaid accounts for 26.5% of total land spending. Considering Medicaid plays a large role in land budgets, states have an interest in cost containment and program integrity. Enrollment and spending increased significantly following implementation of the ACA, simply have moderated in more recent years. While slower caseload growth helped to mitigate Medicaid spending growth in FYs 2018 and 2019, higher costs for prescription drugs, long-term services and supports and behavioral health services, and policy decisions to implement targeted provider rate increases were cited equally factors putting upwards pressures on Medicaid spending.
ix. Medicaid spending is full-bodied on the elderly and people with disabilities
Seniors and people with disabilities make up ane in 4 beneficiaries simply account for almost ii-thirds of Medicaid spending, reflecting loftier per enrollee costs for both acute and long-term care (Figure 9). Medicaid is the primary payer for institutional and community-based long-term services and support – as there is express coverage under Medicare and few affordable options in the private insurance marketplace. Over half of Medicaid spending is attributable to the highest-toll five per centum of enrollees. Withal, on a per-enrollee basis, Medicaid is low-price compared to individual insurance, largely due to lower Medicaid payment rates for providers. Assay shows that if adult Medicaid enrollees had task-based coverage instead, their average health intendance costs would be more than 25% higher. Medicaid spending per enrollee has besides been growing more slowly than private insurance premiums and other health spending benchmarks.
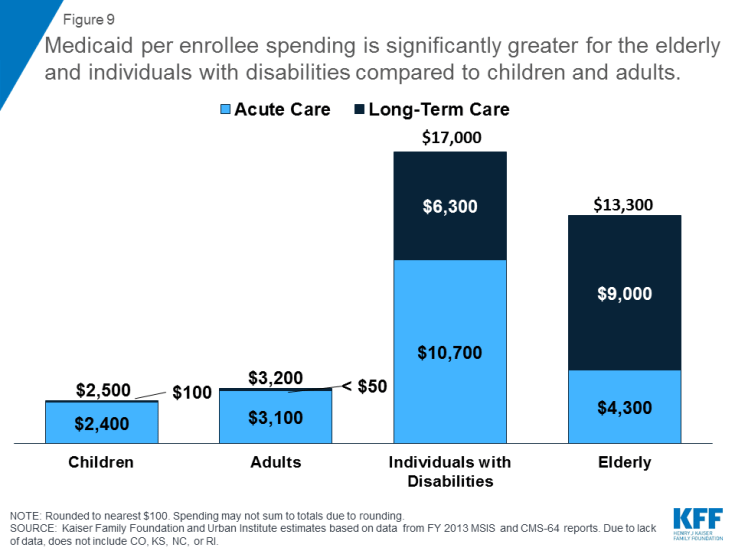
Figure 9: Medicaid per enrollee spending is significantly greater for the elderly and individuals with disabilities compared to children and adults.
10. The majority of the public holds favorable views of Medicaid
Public opinion polling suggests that Medicaid has broad back up. Seven in ten Americans say they have e'er had a connection with Medicaid including three in x who were e'er covered themselves. Even across political parties, majorities accept a favorable opinion of Medicaid and say that the program is working well (Figure x). In addition, polling shows that few Americans want decreases in federal Medicaid funding. In addition to wide-based back up, Medicaid has very strong support among those who are unduly served by Medicaid including children with special wellness care needs, seniors, and people with disabilities.
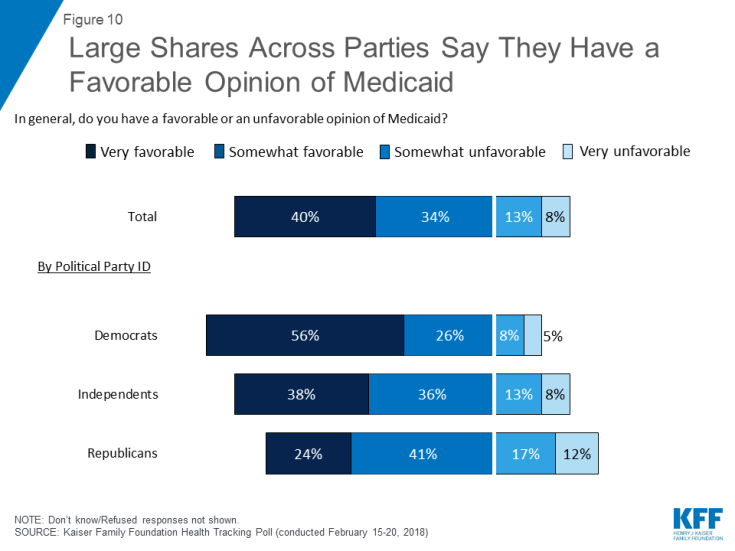
Figure 10: Large Shares Across Parties Say They Accept a Favorable Opinion of Medicaid
Conclusion
Medicaid provides comprehensive coverage and financial protection for millions of Americans, most of whom are in working families. Despite their low income, Medicaid enrollees experience rates of access to care comparable to those amongst people with private coverage. In add-on to acute health intendance, Medicaid covers costly long-term intendance for millions of seniors and people of all ages with disabilities, in both nursing homes and the community. Medicaid bolsters the private insurance market by interim every bit a high-risk pool providing coverage for many uninsured people who were excluded from the private, largely employment-based health insurance arrangement considering of depression income, poor wellness status, or inability. Medicaid also supports Medicare by helping low-income Medicare beneficiaries pay for premiums and cost-sharing and providing long-term services and supports that are not covered by Medicare.
Accounting for ane-fifth of health care spending, Medicaid funding is a major source of back up for hospitals and physicians, nursing homes, and jobs in the health care sector. The guarantee of federal matching funds on an open up-ended basis allows states the flexibility to use Medicaid to address health priorities such as addressing the opioid epidemic. The financing structure also provides support for states to allow Medicaid to operate as safe net when economic shifts and other dynamics crusade coverage needs to grow.
As Medicaid plays a large role in both federal and land budgets and is the primary source of coverage for low-income Americans, it is a abiding source of contend. Efforts to repeal and replace the ACA also included fundamental reforms to Medicaid to cap federal financing through a block grant or per capita cap. Such proposals were narrowly defeated in 2017. Important Medicaid issues to lookout in 2019 include Medicaid expansion developments and continued focus on irresolute the plan through Medicaid demonstration waiver activities, including those focused on piece of work requirements and other eligibility restrictions as well as potential waivers to reshape Medicaid financing. In add-on, other areas in Medicaid to watch are reforms in benefits, payment and delivery systems, efforts to address social determinants of health, efforts to command prescription drug costs, and aggrandize capacity to accost the opioid epidemic and provide community based long-term care services. Congress and states could also consider broader wellness reform that could expand the role of public programs in health care including Medicare for All or Medicaid buy-in programs that could have significant implications for Medicaid.
Source: https://www.kff.org/medicaid/issue-brief/10-things-to-know-about-medicaid-setting-the-facts-straight/
0 Response to "Doctors in Sc Who Accept Family Planning Medicaid"
Postar um comentário